It likely comes as no surprise that what medicine calls “mild traumatic brain injury” (or mTBI, colloquially known as a concussion) are quite common. In fact, some of the people reading this are likely to have experienced at least one mTBI that they were never even aware of, given how common it is for such injuries to go unreported. The actual concrete medical presentation of an mTBI and its associated effects can vary so widely that even medical experts struggle to identify many experiences that can be called common to all mTBIs.
Of course we do know some crucial things. Some of the associated issues include various attentional, cognitive and memory impairments, vertigo, mood disorders, even changes in personality. While some of the symptoms, such as headaches or fatigue may clear within a few days or weeks after the event, others, such as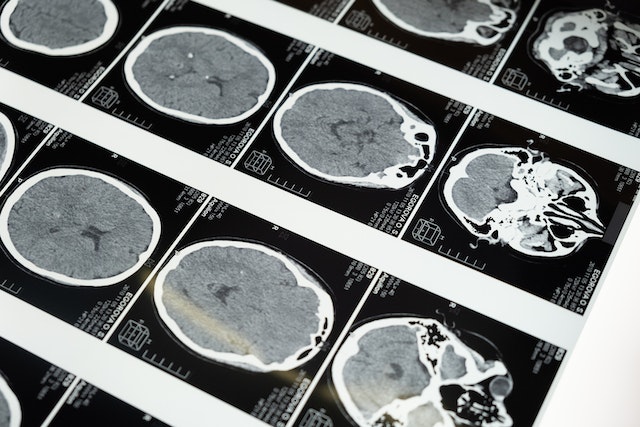 attention, memory and some of the executive functioning issues that are related to organizing, planning and decision making may persist for days, months or even years after the event. The main issue is that in many cases mTBIs have what’s called a “probabilistic distribution” – meaning that there’s no way to accurately predict or determine exactly where the injury to the brain is located. In other words (and please, do not try this at home), you can bonk someone on their skull in the same place, with the same force with the same object and everything else, and wind up with totally different patterns of injury to the brain itself, and it’s often necessary to rely on external manifestations of these symptoms to even guess the location and extent of the damage.
attention, memory and some of the executive functioning issues that are related to organizing, planning and decision making may persist for days, months or even years after the event. The main issue is that in many cases mTBIs have what’s called a “probabilistic distribution” – meaning that there’s no way to accurately predict or determine exactly where the injury to the brain is located. In other words (and please, do not try this at home), you can bonk someone on their skull in the same place, with the same force with the same object and everything else, and wind up with totally different patterns of injury to the brain itself, and it’s often necessary to rely on external manifestations of these symptoms to even guess the location and extent of the damage.
Luckily, and in spite of the complex picture painted above, medical science is also replete with different methods of mitigating or overcoming many of the issues common to the aftermath of mTBI events. For instance, functional medicine physicians (some of them neurologists) work with an array of approaches including nutrition, specific supplements, and other approaches that may use stimulation to help the brain to regain at least part of its functions.
Here at the Sacarin Center: qEEG-based neurofeedback training is one of the avenues that we offer for children and adults with mTBI. Regular readers of our blog may have already learned from our previous article on the basic elements of neurofeedback training and how it helps your electrophysiology to regain the stability and efficiency of brain network hubs and connections known to be related to your specific symptoms. For instance, if attention or executive functioning has been affected, we will create a neurofeedback protocol for your specific presentation which targets the networks that are responsible for retraining and optimizing these skills.
So how is neurofeedback so helpful for mTBIs?
As previously explained, neurofeedback treatment always starts with recording a quantitative electroencephalogram (qEEG), which basically maps out the electrical current at the surface of the skull. From this recording the flow of information through the brain between various areas associated with particular functions can be computed. When using standardized weighted low resolutions electromagnetic tomography analysis (sw LORETA) Neurofeedback, this includes not only cortical but also subcortical levels. As we know from our articles about neural networks, any complex function of the brain is going to depend on the strength of the electrical connection between two areas within it; by comparing the qEEG recording of the injured person to a normative database of healthy brains, we can see where the connections are sub optimal. Thus, when this information is paired with the known manifestations of the symptoms in question, we can integrate all of this information to set relevant “targets” for a neurofeedback treatment protocol to aim for.
You see, the way that neurofeedback (and biofeedback in general) works is a form of operant conditioning – creating an association between a target behavior and a pertinent reward (or consequence). The practitioner is setting up the stage for their client, in a sense, so that their injured brain is electrically encouraged to relearn to behave more like a healthy brain – a bit more abstract, perhaps, than a scientist encouraging a rat to pull a lever by rewarding him or her with a pellet, but in essence the same principle is at work. And studies have shown that, across many different kinds of injuries and many other different approaches to designing qEEG protocols, there is mounting evidence for the benefits to sufferers of mTBIs in reducing the severity and/or persistence of their symptoms.
Dr. Liliana Sacarin herself has for years collaborated with top specialists in the field who are at the forefront of the qEEG swLORETA based neurofeedback training approach when helping individuals with mTBI. If qEEG-based neurofeedback sounds like it could improve your symptoms, reach out and schedule a free consultation with Dr. Sacarin here Liliana Sacarin – TBI Treatment – Seattle, WA
